Radical Cystectomy
Description of Procedure
A radical cystectomy is a major surgery used to treat high-risk bladder cancers, usually muscle invasive bladder cancer. In select circumstances it may be used for superficial but high-risk bladder cancer not amenable to other types of treatment.
In some circumstances, patients will have an increased chance of cure if they receive a course of chemotherapy prior to the surgery (neoadjuvant chemotherapy), in other situation the chemotherapy is best given after surgery (adjuvant chemotherapy). Some patients do not require any chemotherapy at all. This will depend on your particular circumstances.
Here is what to expect once a decision to remove the bladder is made. Print this out to you can check the items off as you proceed through the process.
After Procedure
If you have questions that are not answered here, please contact us.
What to Expect
There is a lot of preparation before this surgery to make sure the surgery and your recovery are as good as possible. YOU MUST BE AN ACTIVE PARTICIPANT TO ENSURE THE BEST POSSIBLE RESULT. Read the information you are given and follow the instructions. Download and read this booklet!
You can watch a video on the ERAS process here.
Pre-operative Imaging
CT Scan - chest, abdomen and pelvis. This has typically been done before the decision to proceed with surgery has been made.
Stoma Marking
APPOINTMENT:
Location: Richmond Hospital North Tower 4th Floor
Your appointment will be arranged for you at the hospital with the stoma nurse. No matter what type of urinary reconstruction you are undergoing (continenent bladder substitute/Studer pouch, catheterizable pouch or ileal conduit/stoma) you will need to see the stoma nurse for marking. The reason is that an ileal conduit is the default type of urinary reconstruction if a Studer pouch or other type of diversion is not possible for technical reasons that are discovered during the surgery. A mark will be placed in the lower abdomen on the RIGHT side and covered with a tape so the mark does not come off.
Making Contact with Ostomy Supply Distributor
Following surgery you will have assistance by home care nursing for the first couple of months with changing of the stoma appliance. The appliance needs to be changed every 3-5 days. Fit of the appliance is very important in ensuring that the stoma and skin remain healthy and that leakage does not occur. Having a trained professional assess your particular situation to obtain the best possible fit is very important. There are many different types of appliances to select from and purchasing supplies without the assessment may not provide the best results (and may cost more because of more frequent replacement).
You will receive a referral to see an ostomy specialist. Ostomy supplies may be eligible for some coverage under Pharmacare - the level will depend on your financial situation.
Nurse Continence Advisor (Optional)
APPOINTMENT:
Location: Richmond Hospital Westminister Health Centre (North-most part of the hospital) in Ambulatory Care. Corey Knott is the NCA.
You do NOT need to see the nurse continence advisor (NCA) if you have decided to have an ileal conduit or stoma procedure. If a decision to have any sort of urinary reconstruction that may require catheterization (e.g. Studer pouch, Mitrofanoff, other) you will need to see our NCA. She will teach you how to catheterize yourself. She will also see you after surgery to ensure you are comfortable with the process of clean intermittent catheterization (CIC).
Pre-Admission Clinic: Anesthesia and Internal Medicine
APPOINTMENT:
Location: Richmond Hospital Pre-operative Assessment Clinic Main Floor North Tower near Radiology
Anesthesia will meet with you a couple of weeks prior to the surgery to ensure that your condition is optimized and to make sure your journey through the operating room is smooth and that your pain is well controlled after surgery. You will have your blood testing done at that time. They will discuss:
Any additional testing necessary to assess your status. For example, specialized They will discuss what is involved with the process of going under anesthesia
What is involved with a general anesthetic. Use of an epidural
Medications. What to continue, stop or any changes
Many patients will also be seen by someone from anesthesia to ensure that your general medical management is optimized on a long term basis and for other specialized testing (e.g. heart or lung function tests).
For You to Do
Your participation is just as important as that of the doctors, nurses and other health professionals involved in your care. Richmond Hospital uses the Enhanced Recovery After Surgery Program (ERAS) to achieve these results. Ensure you have read the patient information booklet on Radical Cystectomy (link is also at the start).
Stop smoking see your family physician for help
Exercise: be in the best shape you can be. Even walking 30 minutes a day will help recovery
Diet: eat a healthy diet. 'Carbohydrate load' an oral nutritional supplement such as 'Boost', 'Ensure' or similar for 1-2 days prior to surgery
Chewing gum: bring sugar free chewing gum to the hospital - chewing gum starting from the night of surgery will help recovery of bowel function
Wash: reduce the chance of infection by washing with soap containing chlorhexiding starting a couple of days prior to surgery. Ask your pharmacist - it is available over the counter without prescription. Examples include Stanhexidine solution, Stanley Chlorhexidine. Shower the night prior to surgery and then wipe down with Chlorhexidine gluconate 2% wipes (SAGE- Antiseptic Body Cleanser).
Sleep: get a good night of rest. Contact your family physician if you need sleeping pills.
Waterproof mattress protector. Accidents with leakage of urine are pretty common after surgery (but will greatly improve over time.
Medic Alert Bracelet with "Cystectomy, Bladder Substitute" if you have a Studer Pouch or "Cystectomy with Ileal Conduit" if you have a condui
Home preparation: think about having your house in order and fridge stocked for when you come home.
Surgery
APPOINTMENT:
Location: Richmond Hospital Admission; You will be called the day prior to surgery for you check in time.
Medications to take the night prior to surgery
FastingNEVER EAT ANY SOLID FOOD OR DRINK ANY FLUID THAT IS NOT CLEAR AFTER MIDNIGHT
You may be asked to drink 1 cup of apple juice the morning of your surgery before coming into hospital
Common mistakes are to eat breakfast, drink coffee or tea, drink non-clear fluids such as orange juice - all of these are strictly prohibited prior to surgery. Failure to follow tese instructions may result in cancellation of your surgery.
How the Surgery is Done
After you go to sleep, the surgery takes between 3-5 hours and is done under a general anesthetic. No matter which type of reconstruction you receive, the cut in the skin is in the lower abdomen below the belly button. The surgery has 2 parts.
PART ONE: radical cystectomy and pelvic lymph node dissection. Radical cystectomy means that the bladder and adjacent organs are removed in order to maximize the chances of cure. The exact details of the surgery may vary based on your specific circumstances. Here is what is removed as part of a radical cystectomy:
Bladder
Adjacent organs: those structures which are in direct contact with the bladder
Males: prostate, sometimes the entire urethra
Females: uterus (to include the cervix and often with the ovaries) and part of the anterior (front) of the vaginal wall
Pelvic lymph nodes
PART TWO: reconstruction of urinary tract. After the bladder is removed, the urine needs to go somewhere. There are many different forms of reconstruction but the 2 most commonly used approaches are:
Ileal conduit – this requires use of a stoma appliance
Orthotopic neobladder – usually the Studer pouch
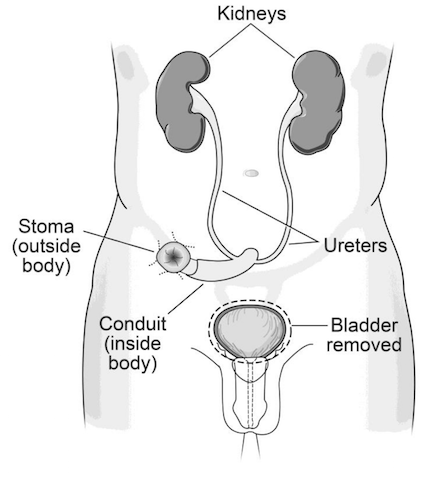
Ileal Conduit
This is the simplest form of urinary reconstruction. The ureters from the kidney are attached to a segement of bowel (specifically, the end of the small bowel - the ilium). That segment of bowel forms the conduit. Continuity in the bowel is re-established by sewing or stapling the cut ends back together. It is the most reliable and least trouble-free type of urinary reconstruction but does require lifelong use of a stoma bag.
The ureters are 'plugged in' to the conduit by seweing them in. Stents (essentially specialized straws/tubes) are placed through anasstomosis (the 'joint') to allow them to heal. The stents are usually removed about 1 week after surgery. Monitoring to ensure that the anastomosis is functioning properly is done with a periodic ultrasound or CT scan. The urine drains continually into a stoma bag which is then emptied through a valve into a container or toilet several times a day. There are many different types of this appliances to match your body shape. An ostomy nurse will help you find one that fits you best. The appliance is then changed by the patient every 5 days or so. This entails pulling the old appliance off, cleaning the skin and placing a new pouch over the stoma. People with ileal conduits and stomas can particiapte in any sort of activity though need to avoid contact sports.
About 1 in 10 people who have an ileal conduit need to have additional surgery for revision. Things like herniation around the stoma (parastomal hernia), scarring where the ureters plug into the conduit (strictures of the anastomosis) or scarring where the conduit exits the body (stomal stenosis) are all potential problems that may arise. Having said that, an ileal conduit is the most trouble-free sort of reconstruction and should strongly be considered if you are very averse to needing additional surgery, higher maintenance or the potential for lifelong catheterization. All types of urinary reconstruction require some maintenance, just like a car. The ileal conduit is the reconstructive version of a Toyota or Honda.
+ Cancer Surveillance
Monitoring for recurrence of cancer is always required following radical cystectomy. The length and intensity of surveillance will vary based on the risk of recurrence.
- Imaging: every 6 months for the first 2 years then yearly thereafter. Usually CT scan
- Blood work: every 6 months for the first 2 years then yearly thereafter. CBC, electrolytes, creatinine, liver function tests. A standing order for blood work will be provided lasting 2 years.
- Cystoscopy: if the urethra was left behind it needs to be checked periodically - usually once yearly
- Assessment by the Urologist indefinitely with every set of imaging and labs (a minimum of twice yearly to start but eventually yearly)
+ Assesement of Conduit Performance
It is important to measure how the conduit is performing even if you think it is working well. Things like obstruction and infection can occur.
- Renal Ultrasound 1-2 months after surgery to check that the kidneys are draining well. After this, routine imaging for cancer surveillance with CT can assess emptying
- Blood tests. You will be asked to go to the public lab (Life Labs or BC Biomedical) to check your blood work periodically in the first few months
Notes on an ileal conduit
- There are almost always teething issues with the conduit at the start. Virtually everyone has an episode at home where the bag comes off and urine leaks all over the bed. You can rest assured that a stoma nurse will work though these issues to find a solution that doesn't leak.
- Medic Alert bracelet. Although rare, some problems with the conduit may incapacitate you such that you cannot communicate to health professionals.
+ Sexual Function
You may be able to continue with sexual activity after having a conduit.
Women may find that the capacity of their vagina is decreased. In these cases, dilation of the vagina may be required. Lubrication is helpful and vaginal estrogen may also help.
Men may loose the ability to achieve natural erections after cystectomy. The reason is that the nerves responsible for erections are attached to the outside of the prostate and bladder. In some circumstances the nerves must be removed to remove all of the cancer. In other cases, preservation of the nerves may be difficult. If preservation of the erection nerves is possible, it may take up to 2 years for erectile reponse to return and it usually requires the use of a medication like Viagra. If you are unable to achieve an erection, intracavernosal injections are always an option. You can read more about these options here. All men permanently loose the ability to ejaculate. While you can still orgasm without ejaculation you will not be able to have children naturally.
Let your urologist know if preservation of fertility is important to you and you can freeze some sperm prior to surgery. Frozen sperm can be used with insemination or in-vitro fertilization.
Studer Pouch
A Studer pouch is one type of a bladder substitute. It is one of the most reliable and commonly performed types of bladder substitutes - also known as 'orthotopic continent bladder replacements'. It allows the patient to empty the bladder through the urethra - that is, it does not require any outside appliances or drainage bags. Aside from the surgical scars, your outward appearance will be the same as it is now.
A Studer pouch is NOT a 'new bladder' and it is critical to understand the important ways in which it differs from a bladder. Not everyone is a candidate for this sort of reconstruction. To be a candidtate you must fulfill every single one of the following requirements:
Agree to lifelong monitoring and followup
Be willing to perform lifelong self catheterization several times per day if it is necessary (see 'Inability to Urinate' below)
Have good hand dexterity
Have good kidney function
Have good liver function
NOT require proton pump inhibitors (these are drugs used for GERD and peptic ulcers)
Have healthy bowel (e.g. no inflammatory bowel disease) *
Have bowel that will reach down to the urethra *
NOT be at high risk for cancer recurrence in the pelvis *
NOT have cancer at the urethral margin *
* Some things are ultimately determined during the surgery. A small fraction of patients who are candidates for a Studer pouch based on pre-operative assessment are found to have reasons why they should not have a Studer pouch during the surgery. As a result, you must be prepared to wake up with an ileal conduit after surgery even though the plan was for a Studer pouch.
How a Studer Pouch is Constructed
A Studer pouch is constructed by taking a longer segment (about 50-55 cm) of small bowel from the ileum. That segment of bowel forms the pouch. Continuity in the bowel is re-established by sewing or stapling the cut ends back together. The isolated segment of bowel is partially opened to create long rectangular sheet which is then folded a couple of times and sewn into a pouch. The ureters are 'plugged in' to the conduit by seweing them in. Stents (essentially, specialized straws/tubes) are placed through anasstomosis (the 'joint') to allow them to heal. The stents are usually removed about 1 week after surgery. The pouch is then hand sewn into the urethra to form an anastomosis. A urethral catheter is placed through the anastomosis. There are multiple 'joins' (anastomoses) - bowel-to-bowel, ureters-to-pouch (x2) and pouch-to-urethra.
Care of the Studer Pouch
Read the following to understand what is involved in its care. In deciding to have a Studer pouch you are consenting to life-long surveillance and maintenance which is much more involved than a conduit to the skin.
When a Studer pouch is working well, it can reasonably replicate what you have with your own bladder - an ability to empty into a toilet through the urethra without any external appliances or bags. Most patients do not need to catheterize and even if you do you will not require an external appliance or bag. The need for additional corrective surgery is higher with a Studer pouch. Up to 30% of patients require further surgical intervention (sometimes minor, but sometimes major). All types of urinary reconstruction require some maintenance, just like a car. A comparison to a car was used for the ileal conduit - which is most like a Toyota/Honda - simple and (mainly) reliable. The car equivament of a Studer pouch is more like a Jaguar - it will drive wonderfully when working but it requires more scheduled and unscheduled service and the service may, at times, be very expensive. A Studer pouch requires more maintenence and participation of the patient than an conduit.
If after reading everything below you feel that this will be too much work, go with the Toyota (ileal conduit), not the Jaguar (Studer pouch).
+ Cancer Surveillance
Monitoring for recurrence of cancer is always required following radical cystectomy. The length and intensity of surveillance will vary based on the risk of recurrence.
- Imaging: every 6 months for the first 2 years then yearly thereafter. Usually CT scan
- Blood work: every 6 months for the first 2 years then yearly thereafter. CBC, electrolytes, creatinine, liver function tests. A standing order for blood work will be provided lasting 2 years.
- Cystoscopy: every 6 months for the first 2 years then yearly thereafter
- Assessment by the Urologist indefinitely with every set of imaging and labs (a minimum of twice yearly to start but eventually yearly)
+ Catheter/Tube Care Immediately After Surgery
When you wake up from surgery there will be a number of tubes in place. The all perform different functions. All will eventually be removed but you will go home with at least 2 of the tubes (the suprapubic and the urethral catheters).
- Ureteral stents: these traverse the anastomosis between the ureters and the pouch. Removed in hospital 5-7 days after surgery.
- Drain tube: this collects any fluid that leaks into the pelvis. Removed 5-7 days after surgery
- Suprapubic cathter: this catheter is one of two that go into the pouch. It ensures that the pouch drains well and allows for the pouch to be flushed. Removed 10-14 days after surgery and only after a cystogram confirms that the pouch is not leaking. The cystogram is done in the hospital and we book it.
- Urethral catheter: this catheter is one of two that go into the pouch. It ensures that the pouch drains well and allows for the pouch to be flushed. Removed 2-3 weeks after surgery by our Nurse Continence Advisor. This is the last tube to be removed and only after at least 2 days have transpired since the suprapubic catheter was removed.
THE CATHETERS GOING INTO THE POUCH (URETHRAL AND SUPRAPUBIC) MUST BE ROUTINELY FLUSHED AFTER SURGERY. The purpose iS to flush out any mucous or blood that may block drainged of urine through the catheters and cause the pouch to rupture. You will be shown how to flush the catheters yourself and home care will visit you once daily
Never attempt to remove the catheters yourself. If a catheter comes out before the scheduled time immediately return to Richmond Hospital for replacement of the tube.
ONLY A UROLOGIST SHOULD REPLACE A URETHRAL CATHETER DURING THE FIRST 2 MONTHS AFTER SURGERY
+ Urination is Different With a Studer Pouch
Remember that the pouch is made from a piece of bowel. It does NOT have the normal nerve supply of a bladder. It does NOT contract/squeeze like a bladder. As a result, your sensation of bladder filling will not be the same as before. How you empty the pouch is different than normal urination and requires practice. Your urologist and the Nurse Continence Advisor will guide you through this process.
Urination in the first 2 months:
- Urinate every 2 hours during the day and every 3 hours at night (set alarm)
- Sit to void initially - eventually males may be able to stand
- Relax the pelvic floor
- Slight abdominal straining
- Hand pressure above the pouch
- Measure the voided volume with a measuring cup once per day
Urination after 2 Months
- Increase the voiding interval from 2 to 4 hours in hourly steps every few weeks
- Measure the voided volume with a measuring cup once per day
- DO NOT EXCEED 500 ML (roughly 16 ounces) VOIDED VOLUME
- Do not worry if you are incontinent as capacity increases. Your continence will improve as the capacity increases. This is because the pressure within the pouch will decrease as it's capacity increases
Notes on Urinary Control with a Studer Pouch
- It takes time for urinary control to return. Do not expect to be dry until the pouch reaches the correct capacity.
- If you become incontinent after being continent/dry, see your urologist to check for a bladder infection and to ensure you are emptying
- Medic Alert bracelet. Although rare, some problems with the pouch may incapacitate you such that you cannot communicate to health professionals. You MUST get a Medic Alert or something similar since from the outside you will look like any other patient.
- MEN: it is more common to have issues with leakage during the day but to be dry at night.
- WOMEN: it is more common to be dry during the day but to leak at night.
+ Inability to Urinate after Studer
About one in four patients will not be able to urinate on a permanent basis after having a Studer pouch. There are a variety of reasons for inability to empty the pouch and every effort will be made to remedy this. If you are still unable to urinate you will be asked to start with clean intermittent catheterization (CIC). Instructions on CIC can be found here.
If you are not willing to risk needing to self catheterize on a long term basis, do not get a Studer Pouch. Go with the ileal conduit.
+ Measurement of Pouch Performance
It is important to measure how the Studer pouch is performing even if you think it is working well. Things like obstruction, infection and derangement of metabolism can occur.
- Renal Ultrasound 1-2 months after surgery to check that the kidneys are draining well. After this, routine imaging for cancer surveillance with CT can assess emptying
- Blood tests. You will be asked to go to the public lab (Life Labs or BC Biomedical) to check your blood work periodically in the first few months
- Checking the amount of urine remaining after you urinate (the Post Void Residual or PVR). There are a few ways that we do this
- Self-catheterize (CIC) and empty into a measuring cup. The nurse continence advisor can will show you how to do this.
- Bladder scan. This is done by the nurse continence advisor with an ultrasound.
+ Metabolic Issues
Remember that the pouch is made from a piece of bowel. It does NOT have the normal urine-proof barrier of a bladder. A normal bladder has an impermeable wall - it does not absorb any fluid, acids or other substances from the urine into the blood stream. The bowel from which a Studer pouch is constructed is capable of absorbing things from the urine - most importantly, acids and salt can be absorbed through the wall of the pouch and into the blood stream. In addition, the bowel secretes mucous (essentially 'snot') - this decreases over time and usually is not a long term issue. All of these issues tend to improve over the first few months but long-term diligence is necessary. Major issues can arise without proper maintenance and monitoring of the pouch.
Metabolic issues: problems and how to avoid them:
- Acid absorption. Urine is usually acidic. It may be absorbed through the pouch. Usually the body can compensate. The absorption of acid will be increased for the first few months after surgery. Acid absorption is also higher if the pouch does not empty completely. When too much acid is absorbed you may feel lethargic, fatigued, have nausea/vomiting and loose your appetite. See your doctor immediately if you have any of these symptoms. To counteract the early effects of acid:
- Bicarbonate. You will need to take some for the first few months. Usually between 2 and 6 grams per day. It comes in a few forms. Choose ONE of these options.
- Sodium bicarbonate. Also known as baking soda. Available in powder form and tablets.
- Sodium Bicarbonate tablets 2 tablets 1-3 times per day (each tablet has about 500 mg of bicarbonate)
- Baking soda 1 tablespoon in water 2 times per day
- Calcium bicarbonate. Tums 2 tablets 2 times per day (each tablet has 500 mg)
- Sodium bicarbonate. Also known as baking soda. Available in powder form and tablets.
- DO NOT TAKE PROTON PUMP INHIBITORS. These medication are used to treat GERD and peptic ulcers. Common types are Prevacid (lansoprazole), omeprazole (Prilosec), esomeprazole (Nexium), dexlansoprazole (Dexilent), rabeprazole (Aciphex). These can trap the acid absorbed through the pouch in your body.
- Bicarbonate. You will need to take some for the first few months. Usually between 2 and 6 grams per day. It comes in a few forms. Choose ONE of these options.
- Dehydration. Ensure that you are drinking 2-3 litres of fluid per day.
- Salt loss. The pouch will loose salt. This is one time where adding salt to your food is a good thing. No need to overdo it.
- Absorption of ammonia. This is generally only a problem if you have liver dysfunction or the pouch is not emptying. Treatment is to drain the pouch properly.
+ Sexual Function
You may be able to continue with sexual activity after having a pouch.
Women may find that the capacity of their vagina is decreased and that leakage may occur with intercourse. In these cases, dilation of the vagina may be required. Lubrication is helpful and vaginal estrogen may also help.
Men may loose the ability to achieve natural erections after cystectomy. The reason is that the nerves responsible for erections are attached to the outside of the prostate and bladder. In some circumstances the nerves must be removed to remove all of the cancer. In other cases, preservation of the nerves may be difficult. If preservation of the erection nerves is possible, it may take up to 2 years for erectile reponse to return and it usually requires the use of a medication like Viagra. If you are unable to achieve an erection, intracavernosal injections are always an option. You can read more about these options here. All men permanently loose the ability to ejaculate. While you can still orgasm without ejaculation you will not be able to have children naturally.
Let your urologist know if preservation of fertility is important to you and you can freeze some sperm prior to surgery. Frozen sperm can be used with insemination or in-vitro fertilization.
Cautions
Seek medical attention (Surgeon, Family Doctor or Emergency Department) if you have any of the following:
Your pain gets worse or does not go away with pain medication
You have a fever over 38.5 C (101 F)
Your incision becomes red, swollen, or hot to touch
You notice alot of clear liqud or foul smelling liquid coming from your incision
You start bleeding from your incision
You feel sick to your stomach (nauseated) or throw up (vomit) often for more than 24 hours
You have diarrhea that lasts for more than 2 days
If you have a drain that is accidentally pulled out
If you are not able to contact your surgeon or family doctor, go to the Emergency Department (Ideally at the hospital where your surgery was done), or call HealthLink BC at 8-1-1 to talk to a registered nurse.
Diet
It might take some time before your appetite returns to normal. To heal, your body will need extra calories, nutrients, and especially protein.
Drink at least 6-8 glasses (2 L) of water each day (1 glass equals 250 mL or 1/4 of a litre)
Eat foods high in protein such as chicken, beef, eggs, tofu, lentils, dried peas, and beans. Dairy products such as mild, yogurt and cheese are also good sources of protein.
Try to eat 5 or 6 small meals throughout the day rather than 3 big meals.
If you are not able to eat enough food each day, you can continue to dring 1 or 2 oral nutrition supplement drinks (e.g. Boost or Ensure) each day.
Caring for your Bowels
Your bowels may not work the same way as they did before your surgery. It may take a few weeks for your bowels to work normally. How to treat constipation:
This can be from your pain medication, especially opioids.
Prevention:
Drink at least 6-8 glasses of water each day
Include fruits, vegetables, dried peas, beans, lentils and whole grains in your diet. These foods are high in feibre.
Keep active. Go for a walk every day.
To treat constipation, talk to your pharmacist about a mild laxative or stool softener.
Activity
Rest is important for your recovery. Try to get at least 8 hours sleep each night. Take naps or rest breaks during the day. Most patients will take 6 weeks off of work following surgery and return to work is often graded for up to 3 months if you do physical activity at work.